Pharmacy teams are less likely to be afraid of reporting dispensing errors since the legal defence for dispensing errors was introduced last April, the findings of a new survey published today (18 December) suggests.
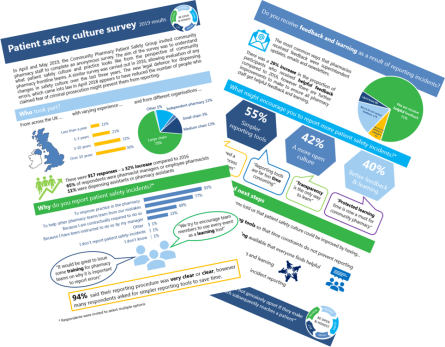
The Community Pharmacy Patient Safety Group (PSG) conducted a survey on patient safety culture in April and May 2019, and invited pharmacy staff from across the UK to participate. This anonymous survey sought to understand patient safety practice from the perspective of frontline pharmacy teams. A similar survey was carried out by Pharmacy Voice in 2016.
Key findings from this year’s survey include:
- The new legal defence for dispensing errors, which came into law in April 2018, appears to have reduced the number of people who claimed fear of criminal prosecution might prevent them from reporting. This figure was 40% in 2016, compared with 22% (internal reporting) and 14% (external reporting) in the 2019 survey.
- 71% of respondents said that they receive helpful feedback after reporting incidents, compared with 55% in 2016. This feedback was given in many different forms, including superintendent updates, newsletters and emails.
- However, 40% of respondents noted that receiving better feedback and learning would encourage them to report more incidents
- 94% of respondents said that current procedures for reporting patient safety incidents are either clear or very clear, however many respondents asked for simpler reporting tools to save time (55%).
Janice Perkins, Chair of the PSG said, “Nurturing an open and honest safety culture in community pharmacies is vital. It requires everyone to feel confident in openly sharing when things go wrong to learn from errors and prevent them occurring again. Community pharmacies deliver incredibly safe care. However, it will never be possible to eliminate all patient safety incidents in health settings, including pharmacies.
“These results demonstrate that there have been significant positive improvements since 2016. However, participants also highlighted particular areas where more could be done, such as simpler reporting tools. We also want to ensure that all members of the pharmacy team receive helpful feedback and learning when things go wrong.
“The patient safety group is committed to continuing its work at a national level to influence changes in policy and regulation that will help to improve safety by encouraging more reporting of incidents and improving feedback and learning.”
The PSG has used the survey’s findings to develop a new discussion tool for all pharmacy teams. This handy resource helps teams have an open conversation about their safety culture and reflect and review on what improvements could be made.
Community pharmacy teams are an essential and integral part of the health and care landscape and provide safe and effective care to the patients they serve, through the dispensing of medicines as well as the provision of health advice and clinical services.
Safety culture assessment tool
In 2016 the group have also worked closely with the primary care team from the Greater Manchester Patient Safety Translational Research Centre (GM PSTRC) to further develop their Manchester Patient Safety Framework (MaPSaF), which was produced to help healthcare teams reflect on their progress in developing a patient safety culture and managing risks to patient safety.
This tool is designed to help community pharmacy teams understand their stage of development with regards to the importance they place on patient safety. The MaPSaF is used regularly in other primary care settings, such as general practice, and Pharmacy Voice’s Patient Safety Group has worked with the GM PSTRC team to help make it a more user-friendly and accessible tool for community pharmacy teams and organisations.
The community pharmacy MaPSaF was developed by Darren Ashcroft, Charles Morecroft, Dianne Parker and Peter Noyce at the University of Manchester as part of a project that was funded by the Community Pharmacy Research Consortium. The original framework was developed by Dianne Parker, Tanya Claridge, Sue Kirk, Aneez Esmail and Martin Marshall supported by the National Primary Care Research and Development Centre, University of Manchester.